
LGBT

Whenever I’m asked what health equity means for my work at Tides, I think about the moments in my life that have shaped my understanding of class, race, and equity, and that fuel the work I do today. Growing up, I remember helping my mother pack up her classroom at the beginning of each summer break. Each afternoon, we would drive from her school in a low-income, south central Los Angeles neighborhood to the middle-class west Los Angeles community that we called home. With eyes fixed on the activity flashing by, I would press my forehead against the glass and observe the stark changes in the environment as we traveled west. The houses changed; they became more colorful and better maintained. The streets changed; they became cleaner, better-lit, and offered more sidewalk space. The accessible food sources changed; there were more supermarkets, fewer fast food chains, and fewer liquor stores. Even the population changed; there were fewer people of color—fewer people who looked like me.
As a young child, the juxtaposition of these environments served as my first introduction to privilege and the reality of inequity. It would certainly not be my last.
To build towards a world in which every person has the opportunity to attain their full health potential, we must reinvent the way we are approaching the work, break out of our sectoral silos, and collaborate to develop intersectional solutions.
With a background in public health, focused on health policy and management, I am interested in how our systems, policies, and traditional approaches can be changed to promote health equity and eliminate the stark differences in access, quality, and environmental conditions by zip code. I often think about what it will take to truly achieve health equity and how it can improve the lives of children, families, and entire communities. The Center for Disease Control and Prevention describes health equity as a state in which all people have the opportunity to attain their full health potential, and no one is disadvantaged from achieving this potential due to socially determined circumstances. Health inequities also show up as life quality and expectancy, rates and severity of disease, and access to treatment, all of which vary based on socio-economic status. [efn_note] https://www.cdc.gov/chronicdisease/healthequity/index.htm [/efn_note]
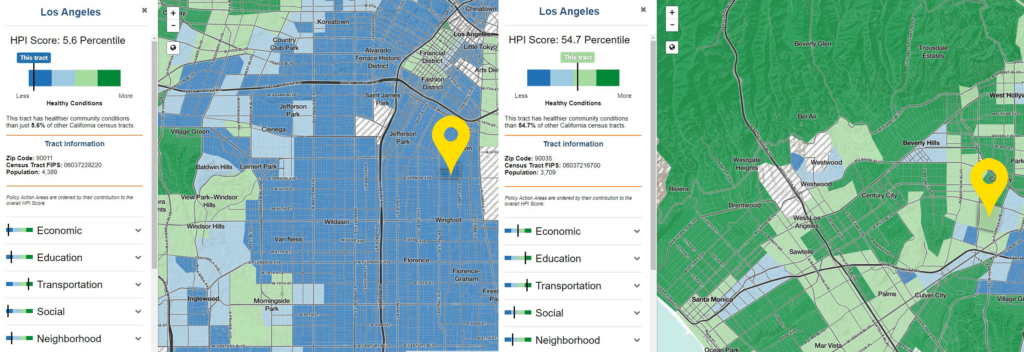
Above: Healthy Places Index (HPI) assign a census tract score based on community, economic, health, and education conditions. The percentile indicates what percentage of California census tracts had poorer conditions than the represented track. Left: my mother’s school’s tract score (5.6); Right: my childhood neighborhood score (54.7). Below: A comparison of the stark differences in the Healthy Places Index (HPI) between the two neighborhoods.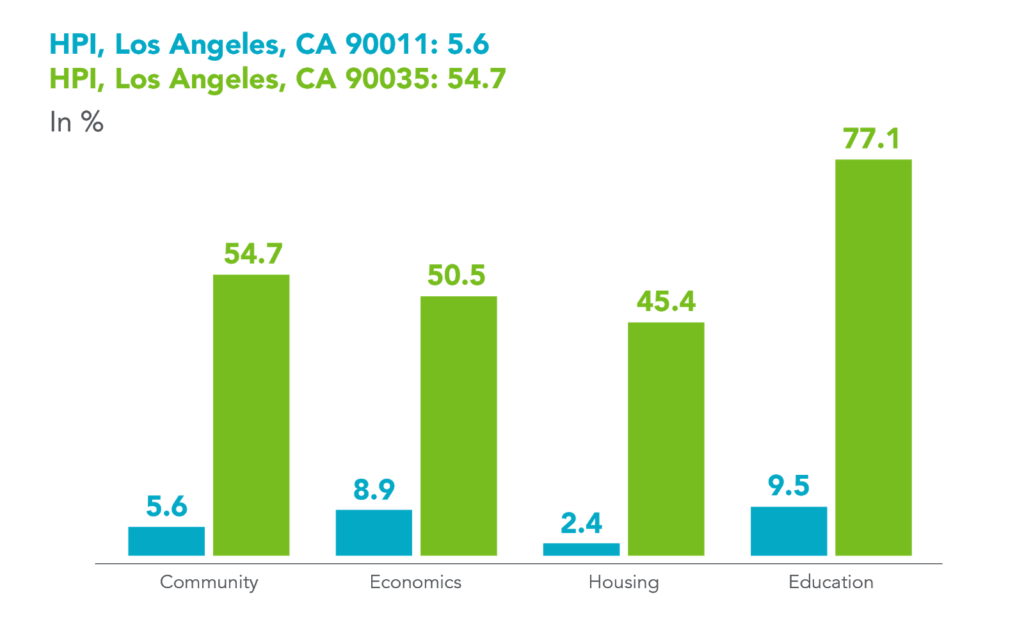 All Hands on Deck for Health Equity
All Hands on Deck for Health Equity
Health equity is essential to an equitable society, yet the path toward its achievement comes with significant obstacles. Baseline challenges of poverty and discrimination are powerful forces that are too large for a single organization or sector to successfully address in a vacuum. Health status isn’t clear-cut and is influenced by intersecting factors, including quality of and access to housing, education, transportation, income, and employment. Consequently, effective solutions to health inequities must incorporate diverse sectors, which historically have functioned in silos. To build towards a world in which every person has the opportunity to attain their full health potential, we must reinvent the way we are approaching the work, break out of our sectoral silos, and collaborate to develop intersectional solutions.  The benefits of collaboration have been well-documented through research and practice. The Journal of Public Health Medicine and Practice explored the perceived benefits of collaboration between local health departments, schools, and programs of public health, and found that collaborative efforts are mutually beneficial and valuable for transforming public health practice, education, and research.[efn_note] https://www.ncbi.nlm.nih.gov/pubmed/29927902 [/efn_note] The American Public Health Association also highlighted the important role of cross-sector collaboration between public health, healthcare, community development, and other fields to reduce health inequities.[efn_note] https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2017/01/17/opportunities-for-health-collaboration [/efn_note] More broadly, collaboration between organizations and across sectors presents opportunities such as:
The benefits of collaboration have been well-documented through research and practice. The Journal of Public Health Medicine and Practice explored the perceived benefits of collaboration between local health departments, schools, and programs of public health, and found that collaborative efforts are mutually beneficial and valuable for transforming public health practice, education, and research.[efn_note] https://www.ncbi.nlm.nih.gov/pubmed/29927902 [/efn_note] The American Public Health Association also highlighted the important role of cross-sector collaboration between public health, healthcare, community development, and other fields to reduce health inequities.[efn_note] https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2017/01/17/opportunities-for-health-collaboration [/efn_note] More broadly, collaboration between organizations and across sectors presents opportunities such as:
Leveraging collaborative partnerships across sectors and its associated benefits better positions the overall field to move the needle on health equity issues by more effectively addressing the range of intersecting factors that influence them.
Tide’s Role In Amplifying Collaboration to Advance Health Equity
As nonprofit leaders recognize the benefits of collaborative work across sectors, new initiatives are emerging for health equity-focused organizations and leaders to build relationships, share resources, and set the foundation for collaborative work. In partnership with the Robert Wood Johnson Foundation (RWJF), Tides recently launched Policy Connect, a pilot initiative designed to support a cohort of grantees in coordinating their policy work to advance the health and well-being of all children and families. The initiative was created in direct response to grantees’ expressed need to connect with one another and further elevate the work and resources that are critical to advancing their shared vision.
Leveraging collaborative partnerships across sectors and its associated benefits better positions the overall field to move the needle on health equity issues by more effectively addressing the range of intersecting factors that influence them.
Since its formal launch in June 2019, Policy Connect has created a space for grantee members to participate in a range of activities designed to support sharing resources and learnings, building deeper relationships, and advancing collective work. To inform the initiative design process, RWJF and the Tides team formed an Advisory Group, which included leaders from seven RWJF Healthy Children and Families (HCF) grantee organizations to help co-design a coordination strategy, provide input on activities and resource needs, and develop short-term outcomes for the initiative.
Since its inception, Policy Connect has provided:
Though the Policy Connect initiative is still in its pilot phase, members have already begun to experience some benefits of multi-sector or cross-organization collaboration. My team and I have observed that members share more information and resources, strengthen relationships with peers, gain access to diverse networks and individuals, align strategy, and support one another to identify and pursue policy opportunities. Among other successes, two grantee members collaborated to incorporate low-wage worker’s stories into a recent Washington Post opinion piece describing the inadequacy of many working-class jobs and critically assessing the impact of policies like Public Charge.
Looking Ahead: The Role of Philanthropy
Through my involvement in the Policy Connect pilot initiative, I have seen the powerful role that collaboration can play in cultivating more effective and aligned strategies to advance towards health equity. I have grown more confident that we can collectively work to move the needle on social determinants of health and eventually get to a place where everyone has the opportunity to achieve health, no matter what zip code they live in. Now, I think of my childhood car rides between my mother’s school and our home through a health equity lens, and I see collaboration as a tool for leveling the playing field for children and families across the country.
Philanthropy must commit to playing a more significant role in creating intentional environments in which collaborative work can emerge.
To make this vision a reality, philanthropy must commit to playing a more significant role in creating intentional environments in which collaborative work can emerge. Given that foundations are well connected to a broad cohort of grantee organizations and know the work, resources, and needs that exist across sectors, they are well-positioned to connect grantees to resources within their portfolios and create learning communities that promote resource sharing. Philanthropic organizations can make their investments in health equity efforts go further if they also invest in collaborative initiatives that help their funded grantees build relationships, share resources, brainstorm ideas, and collaborate. Such opportunities will strengthen the work of each individual grantee organization, reduce duplicative efforts, and enhance the collective impact of the field.
As a next step, philanthropic organizations can begin to think more strategically about how the organizations that they fund connect. What do they have in common in terms of location, strategy, population served, type of work, mission, and goals? What capacity or information gaps exist that other funded organizations might be able to address? The field should work to fund and create more opportunities for grantee organizations with similar goals or mutually beneficial strengths to connect and co-create solutions for the complex and intersecting issues that they face. Working in collaboration, we can achieve shared health equity goals.

LGBT

Corporate Partners

Philanthropy

Read the stories and hear the voices of social change leaders fighting for justice.